Placing Patients at the Center of Health Care

Longstanding debate about how to ensure and measure excellent healthcare abounds. Increasingly health professionals, insurers, researchers and, indeed, patients and families, are recognizing that health care is better when patients’ needs are placed at the center of the decision-making process.
How can we capture patient voices in ways that can improve healthcare delivery, cost, and outcomes? How do we measure what matters to the person who becomes a patient when illness strikes? These questions are the focus of much of AIR’s work in health care.
Patient-Reported Outcomes
The ultimate objective of medical care is not only to prolong life but to relieve suffering and improve functioning. The measurement of suffering and daily functioning cannot occur without data provided directly from patients. While patient reports of how they feel and what they are able to do are solicited within the clinical interview, “Patient-Reported Outcome (PROs)” or “Patient-Reported Outcome Measures (PROMs)” offer the opportunity to systematically quantify those reports into data; thus, allowing medical evidence that includes the patients’ voice.
PROs take the answers patients give to questions and turn them into scores on dimensions of health such as pain, fatigue, emotional distress, and physical functioning. PROs are designed to measure health based on person reports at the population and clinic levels and enable comparisons across sub-populations defined by age, ethnicity, gender, disease, treatment (and other variables) both at a single point in time, and according to change over time. PROs describe patients’ experiences as they deal with acute or chronic diseases or conditions and as they undergo treatment or are participating in a clinical trial.
Patient-Reported Outcomes Measurement Information System (PROMIS) Network Center
Patient-Reported Outcome Performance Measures (PRO-PMs) are the use of PROs to measure the performance of a healthcare provider or system. Medicare, Medicaid, and private insurers are testing the use of PRO-PMs to describe the value of the services that they pay for. AIR was a Center of Excellence for the development of NIH’s Patient-Reported Outcome Measurement System, a sophisticated, automated catalog of PRO measures AIR developed a PRO measurement system for individuals suffering from a rare disease.
Better Understanding Sickle Cell Patients’ Health-Related Quality of Life
Scientific breakthroughs in detecting and treating rare diseases are expanding life expectancies for individuals in unprecedented ways. Our researchers developed a Sickle Cell Disease Patient-Reported Outcome measurement system called ASCQ-Me that helps bridge the gaps in understanding about adult patients’ experiences and long-term needs.
 What Is the Value of Patient-Reported Outcomes?
What Is the Value of Patient-Reported Outcomes?
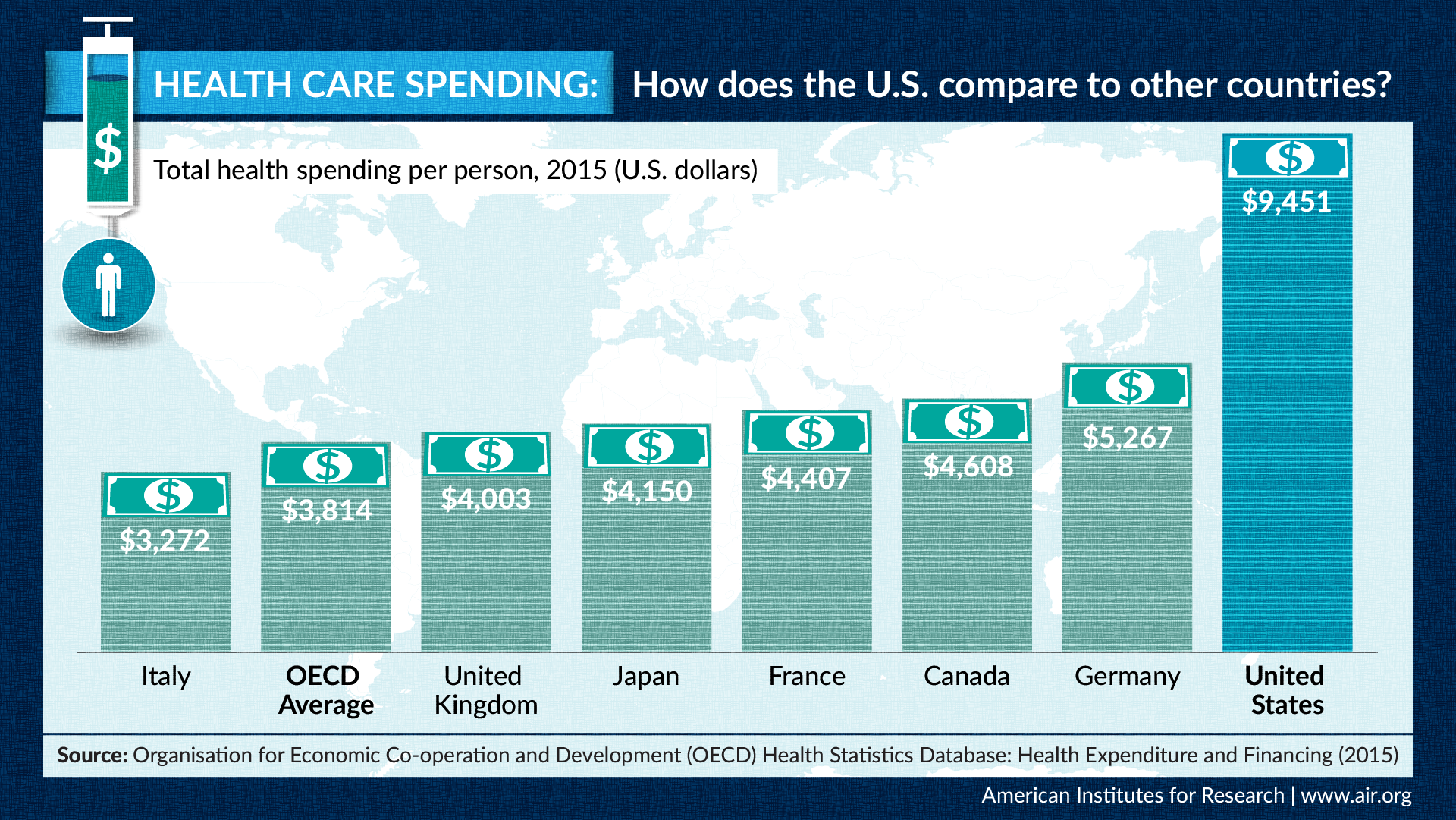
As the infographic below shows, the U.S. spends more on health care compared to other industrialized nations, despite Americans having poor health outcomes. Patient-reported outcomes measure patients’ direct experiences of their health condition and health care. In this video, San Keller explains the value of such outcomes in promoting public health and improving the quality of health care.
Patient-Centered Measurement
Patient-centered measurement involves partnering with patients in a meaningful way to decide what we measure, how we measure it, and how we report and use the results of measurement.
Five Principles to Guide Patient-Centered Measurement
AIR's Center for Patient and Consumer Engagement developed these principles to inform a vision of health care measurement that reflects what patients say they need and want. The principles are:
- Patient-driven - Patients’ goals, preferences, and priorities drive what is measured and how performance is assessed.
- Holistic - Measurement recognizes that patients are whole people and considers their circumstances, life and health histories, and experiences within and outside of the health care system.
- Transparent - Patients have access to the same data as other stakeholders and understand how data are used to inform decision-making around care practices and policies.
- Comprehensible & Timely - Patients and other stakeholders get timely, easy-to-understand data to inform decision-making and quality improvement.
- Co-created - Patients are equal partners in measure development and have decision-making authority about how data are collected, reported, and used.
Describing the Quality of Cancer Care from the Patient’s Point of View
 The CAHPS® Cancer Care Survey is the first Consumer Assessment of Healthcare Providers and Systems (CAHPS) Survey designed for a specific illness. Created by AIR and the Mayo Clinic, it assesses the experiences of adults receiving cancer treatment in outpatient and inpatient settings, including independent community oncology practices, cancer centers at community hospitals and cancer centers at academic medical centers (including those designated as comprehensive cancer centers by the National Cancer Institute (NCI)). The survey’s three instruments, available in English and Spanish, correspond to the major treatment modalities: radiation oncology, medical oncology, and cancer surgery. They build on the CAHPS Clinician & Group Survey to capture cancer care features that are important to patients and for which patients are the best source of information.
The CAHPS® Cancer Care Survey is the first Consumer Assessment of Healthcare Providers and Systems (CAHPS) Survey designed for a specific illness. Created by AIR and the Mayo Clinic, it assesses the experiences of adults receiving cancer treatment in outpatient and inpatient settings, including independent community oncology practices, cancer centers at community hospitals and cancer centers at academic medical centers (including those designated as comprehensive cancer centers by the National Cancer Institute (NCI)). The survey’s three instruments, available in English and Spanish, correspond to the major treatment modalities: radiation oncology, medical oncology, and cancer surgery. They build on the CAHPS Clinician & Group Survey to capture cancer care features that are important to patients and for which patients are the best source of information.
The survey is used to improve the patient-centered focus of cancer centers, oncology practices, hospitals, and health systems. Results can also inform decisions made by providers, patients and their families; accrediting organizations, and payers.
Measuring the Quality of Care Coordination in Primary Care
With funding from the Agency for Healthcare Research and Quality (AHRQ) AIR led a team of researchers to develop a measure of coordination of care for adults in primary care settings. The Care Coordination Quality Measure for Primary Care (CCQM-PC), based on CAHPS methodology, can be used as a quality improvement, accountability, and research tool.
