The Quest to Connect Patient and Family Engagement to Health Care Quality and Safety
Everyone wants safe, high-quality health care. Many in the field realize that health care professionals alone cannot make health care better. Another partner is critical: patients and families.
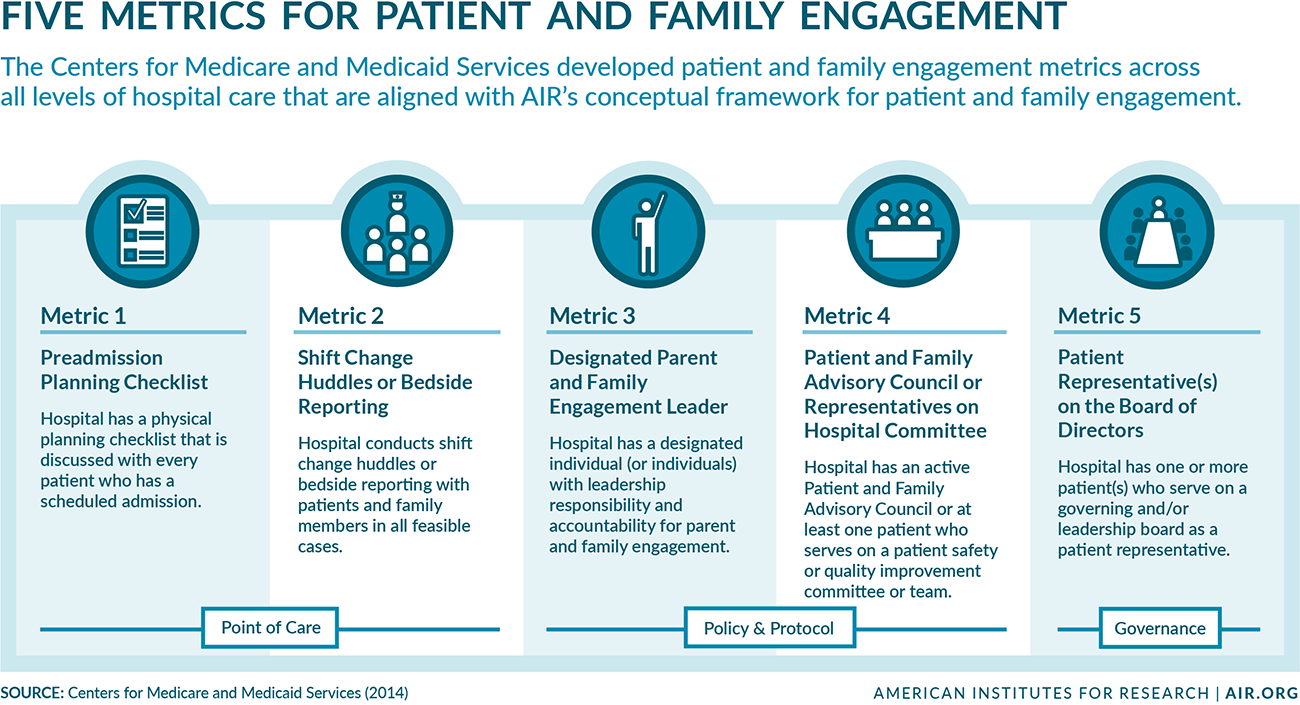
Patient and family engagement is “persons, families, their representatives, and health professionals (clinicians, staff, and leaders), working in active partnership at various levels—point of care; organizational design, policy and procedure; organizational governance; and community/policy making—across the health care system and in collaboration with communities to improve health, health care, and health equity.”
—A 2013 Health Affairs article by AIR and the definition used in all AIR patient and family engagement projects
AIR has been a leader in the evolution of patient and family engagement as a key quality improvement strategy. Through a published conceptual model, a hospital guide, and a nationwide convening to develop the country’s first roadmap for practice and research, AIR experts have provided hospitals and health care systems with practical and proven approaches to integrate the perspectives and ideas of patients and families in the push to improve care.
AIR serves as a contractor for a patient and family engagement initiative that involves more than 4,000 hospitals in 16 regional and national Hospital Improvement Innovation Networks. This initiative, funded by the Centers for Medicare and Medicaid Services (CMS), has already led to incredible changes: A December 2016 Health & Human Services (HHS) Department report showed that hospital-acquired conditions dropped 21 percent over a five-year period, resulting in 2.1 million people avoiding a hospital-related harm, and saving $28 billion in care costs between 2010 and 2015. Now in its ninth year, the program has moved that needle much further, resulting in 8,000 lives saved and $2.9 billion in additional cost savings between 2014 and 2016, according to a 2018 HHS report.
Thomas Workman, principal researcher at AIR, serves as a senior advisor to the CMS initiative and AIR’s own Center for Patient and Consumer Engagement. In this Q&A, he shares his insights about the current state of health care safety and patient and family engagement—and where we’re headed.
Q. What exactly is patient and family engagement?
Workman: Patients and families can become active partners to doctors, nurses, health care systems, hospitals, and clinics when they ask questions about their care. They also can become active partners behind the scenes, getting involved in decisions about policies and procedures, helping to solve a problem like hospital-acquired infections, considering a new medical service or technology, or even becoming part of a hospital’s governance.
Encouraging patients and family members to become partners in their own care can have a direct impact on their own outcomes—and other patients’ as well. Patients and families can share experiences, insights, perspectives, and ideas that make a significant difference in a hospital’s decisions and success.
CMS developed five metrics that reflect the conceptual model of patient and family engagement created by AIR.
Q. What challenges do hospitals face in engaging patients and families as partners in improving quality and safety?
Workman: The idea of partnering with patients is quite new, and old paradigms die hard. Traditional health care has always been centered on treating patients, but it has not been patient-centered. In other words, patient experience—from accessing and paying for treatment to receiving care to the emotional experience of illness—has not been the driving factor in designing or operating health care services. Health care has always been done to or for the patient rather than with the patient. As a result, patients haven’t traditionally asked questions or become involved in decisions about their care, much less how a hospital provides care to others or fixing problems they’ve experienced with health care.
One of the biggest challenges for hospitals is overcoming myths about patient and family advisors. One myth is that patient advisors don’t understand the complexities of health care and will ask for things that are unreasonable or impossible. Another is that informing them takes too much time and, once they get the information, they’ll share it inappropriately. Patient and family advisors have had to prove their intentions, their insight, and their ability to keep sensitive information confidential.
At the same time, hospitals have had to learn how to recruit and select patient and family advisors, provide effective onboarding and mentoring, and involve advisors in the governance process in a way that their contributions are relevant and efficient. AIR creates and distributes knowledge, tools, and resources to help hospitals and patient and family advisors work together successfully.
Hospitals that have fully embraced patient and family engagement have seen a variety of positive outcomes, from reduced litigation to improved patient experience scores. Several studies have even found reduced turnover and increased job satisfaction among clinical staff.
Q: Is there a specific link between patient and family engagement and improvements in quality and safety?
Workman: We think there is—but building this case from statistics alone is challenging. Analyses done by AIR and many hospital networks themselves seem to suggest that there is a relationship between hospitals that implement patient and family engagement metrics and the improvement rates of their quality and safety measures. Hospitals that met four or five of the CMS metrics have seen reductions in their hospital-acquired infection rates, injury rates from falls, and preventable readmissions.
As part of our work on the CMS project, AIR is conducting case studies of participating hospitals that have seen improvements and those that have not. We want to better understand whether the ways in which the patient and family engagement metrics are applied to quality and safety makes a difference. Our goal is to identify which specific applications impact quality and safety.
Q. What’s the future of patient and family engagement?
Workman: We’re done defining. We’re done conceptualizing. We’re done even arguing about how wonderful or terrible engaging patients and families in health care is. There are now 4,000 hospitals working to engage patients and families, which is pretty astonishing.
Where we’re headed is validation that the metrics of patient and family engagement are a direct contributor to quality and safety. There is also more work to be done in unifying these efforts across different health care settings, such as ambulatory care, rehabilitation centers, dialysis centers, and nursing homes—particularly in the transition of care from one facility to another. CMS has reorganized its funding structure to encourage this broader approach, and there will be a need for new and different approaches and tools to help systems and patient and family advisors to partner at this level.