Understanding Patients’ Feelings on COVID-19 Vaccinations and Addressing Vaccine Hesitancy
With three COVID-19 vaccines approved for emergency use authorization in the U.S., vaccine acceptance among the public is critical to curtailing the pandemic. Despite promising vaccine trial data, some individuals, particularly Black Americans and people living in rural areas, remain hesitant to be vaccinated against COVID-19.
For instance, about four in 10 Black men and women said they would like to “wait and see” how the vaccine works for others before getting vaccinated themselves, a survey by the Kaiser Family Foundation found. Further, almost 20 percent of Black women said they would “definitely not” get vaccinated against COVID-19 when the vaccine becomes available to them. The same analysis found that individuals living in rural communities had some of the highest vaccine hesitancy rates, with 35 percent reporting that they will either “probably not” or “definitely not” get the COVID-19 vaccine when it becomes available to them.
- Conducted between Oct. 1 and Oct. 20, 2020
- 1,016 adults age 18 and older residing in the U.S.
- Used the Ipsos KnowledgePanel®
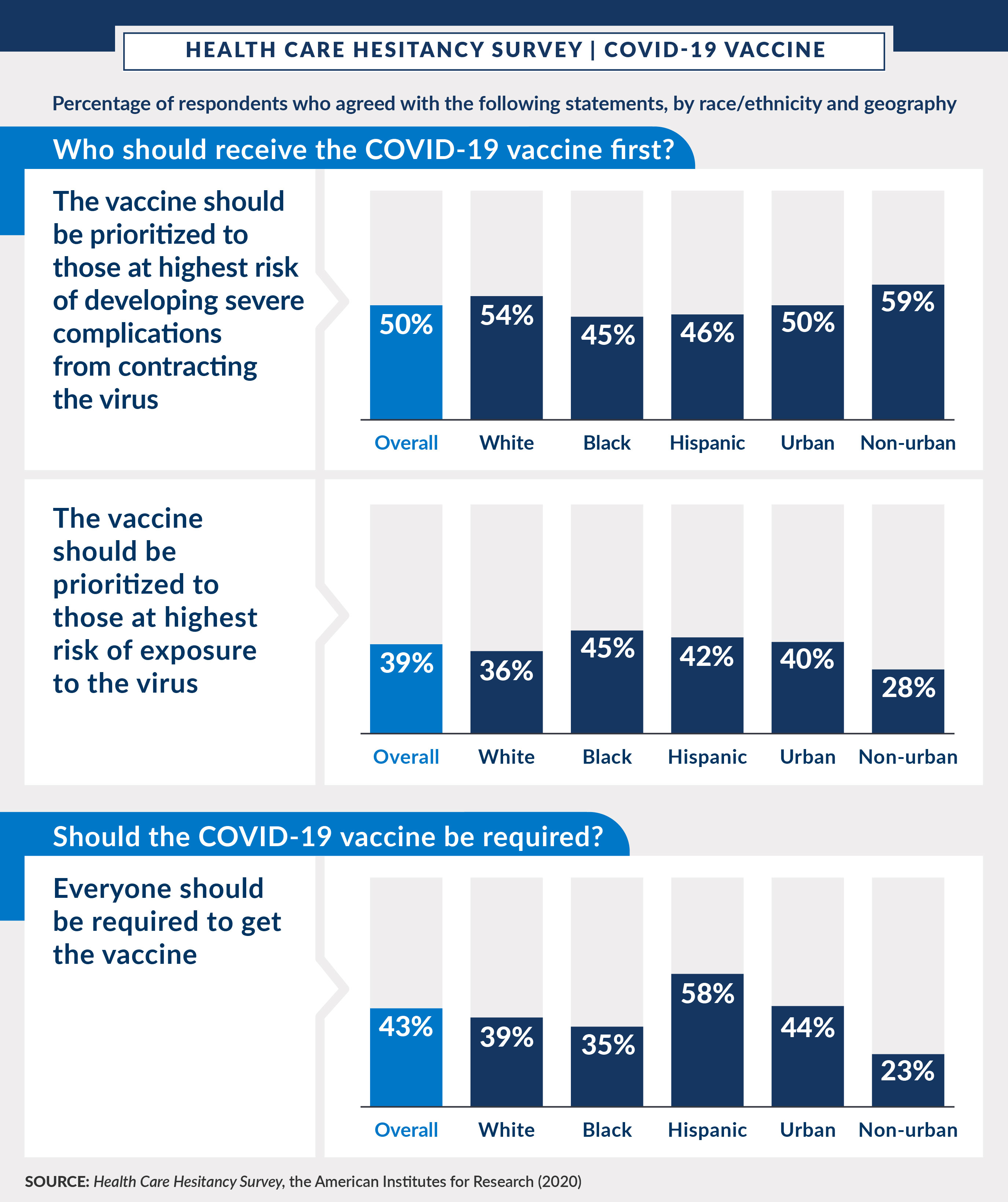
A nationally representative survey from the American Institutes for Research provides additional data on how the public feels about vaccine access, prioritization, and requirements.
What Does the Public Think About COVID-19 Vaccines?
Findings from AIR’s survey provide valuable insights about what prevents individuals from seeking care, including vaccinations, during the pandemic and what might make them more comfortable doing so. Health care providers and policymakers can use these findings to take steps to encourage more people to receive needed health services, like a COVID-19 vaccine, during this time. The survey findings provide three primary takeaways on public opinion regarding COVID-19 vaccines.
Opinions on who should receive the vaccination first vary based on race/ethnicity. Half of all respondents agreed that those at highest risk of developing severe complications from contracting the virus should be prioritized to receive a COVID-19 vaccine. A greater number of white respondents (54 percent) than Black and Hispanic respondents (45 percent and 46 percent, respectively) agreed that vaccines should be prioritized for those with highest risk of developing severe complications. Respondents living in urban areas had higher levels of agreement with this prioritization (59 percent), compared with half of non-urban respondents.
Respondents are also split on whether people with a high risk of contracting COVID-19 should receive priority status for vaccines. Almost 40 percent of respondents agreed that those at highest risk of exposure to the virus should be prioritized to receive a vaccine. A greater number of Black and Hispanic respondents (45 percent and 42 percent, respectively) agreed with this prioritization, compared with 36 percent of white respondents. The lowest level of agreement with prioritization to those at highest risk of exposure was among non-urban residents (28 percent), compared with 40 percent of urban residents.
Some respondents believe that a COVID-19 vaccination should be required. The survey also asked respondents about their level of agreement regarding a vaccine requirement. About two-fifths (43 percent) of all respondents thought everyone should be required to get the COVID-19 vaccine. The highest level of agreement was among Hispanic respondents (58 percent), compared with white respondents (39 percent) and Black respondents (35 percent). The lowest level of agreement was among non-urban residents (23 percent), compared with 44 percent of urban residents.
Implications of Vaccine Hesitancy and How to Improve Vaccine Acceptance
The survey’s findings demonstrate the need for evidence-based patient education about the importance of vaccine implementation and vaccine safety, particularly among specific populations. Data from 23 states show that Black Americans are receiving COVID-19 vaccines at significantly lower rates than white Americans. Lower vaccination rates in communities of color are particularly concerning because the disease burden of COVID-19 has been greater in these communities. For example, Black Americans are at higher risk for severe disease and death due to COVID-19. To address such racial/ethnic health disparities, public health stakeholders and policymakers should consider focusing on increasing vaccination rates in communities of color.
It is equally important to tailor community outreach and education on vaccine acceptance to address specific community concerns. For example, some of the barriers to vaccine acceptance in Black communities may be tied to longstanding mistrust in the health care system and clinical research. It is critical that officials recognize this mistrust and directly address community concerns.
Vaccine acceptance will be both a collaborative effort and one that will help control the COVID-19 pandemic by maximizing the benefits of the vaccine. By working side by side with communities, officials can help address COVID-19 disease disparities, while working toward the common goal of ending the pandemic and returning to normal life.
